Overcoming Baseball Injuries: Essential Tips for Faster Recovery and Unstoppable Performance
Intro to Baseball Injuries
Baseball is a popular sport enjoyed by millions of people worldwide. However, like any physical activity, it comes with its own set of risks and potential injuries due to the nature of the sport. This article will discuss common baseball injuries, sports physical therapy interventions, and strategies to decrease the likelihood of injury and rehabilitation techniques.
Common Baseball Injuries
Labral Tears
The labrum is a ring of cartilage that lines the shoulder socket (glenoid), providing stability and cushioning for the joint. In baseball players, particularly pitchers, the high forces placed on the shoulder during the throwing motion can lead to labral tears. There are different types of labral tears, including SLAP (Superior Labrum Anterior to Posterior) tears and Bankart lesions.
Symptoms: A labral tear can cause pain, a catching or grinding sensation in the shoulder, instability, and loss of strength or range of motion in the affected shoulder. In some cases, athletes may experience a feeling of the shoulder "giving out" or "slipping."
Recovery: The recovery time for a labral tear depends on the severity of the injury and the chosen treatment approach. With conservative treatment, most athletes can expect to return to their sport within several weeks to months, depending on their adherence to the rehabilitation program and the resolution of symptoms. Recovery from arthroscopic surgery can take several months, with a gradual return to throwing and sports-specific drills.
Rotator Cuff Injuries
The rotator cuff is a group of four muscles and tendons (supraspinatus, infraspinatus, teres minor, and subscapularis) that surround and stabilize the shoulder joint. Baseball players, especially pitchers, are susceptible to rotator cuff injuries due to the repetitive overhead throwing motion.
Symptoms: Rotator cuff injuries can range from mild inflammation (tendinitis) to partial or complete tears of the rotator cuff tendons. Symptoms may include shoulder pain, particularly during overhead activities, weakness, and loss of range of motion. A complete tear may cause a sudden, sharp pain accompanied by a "pop" sensation.
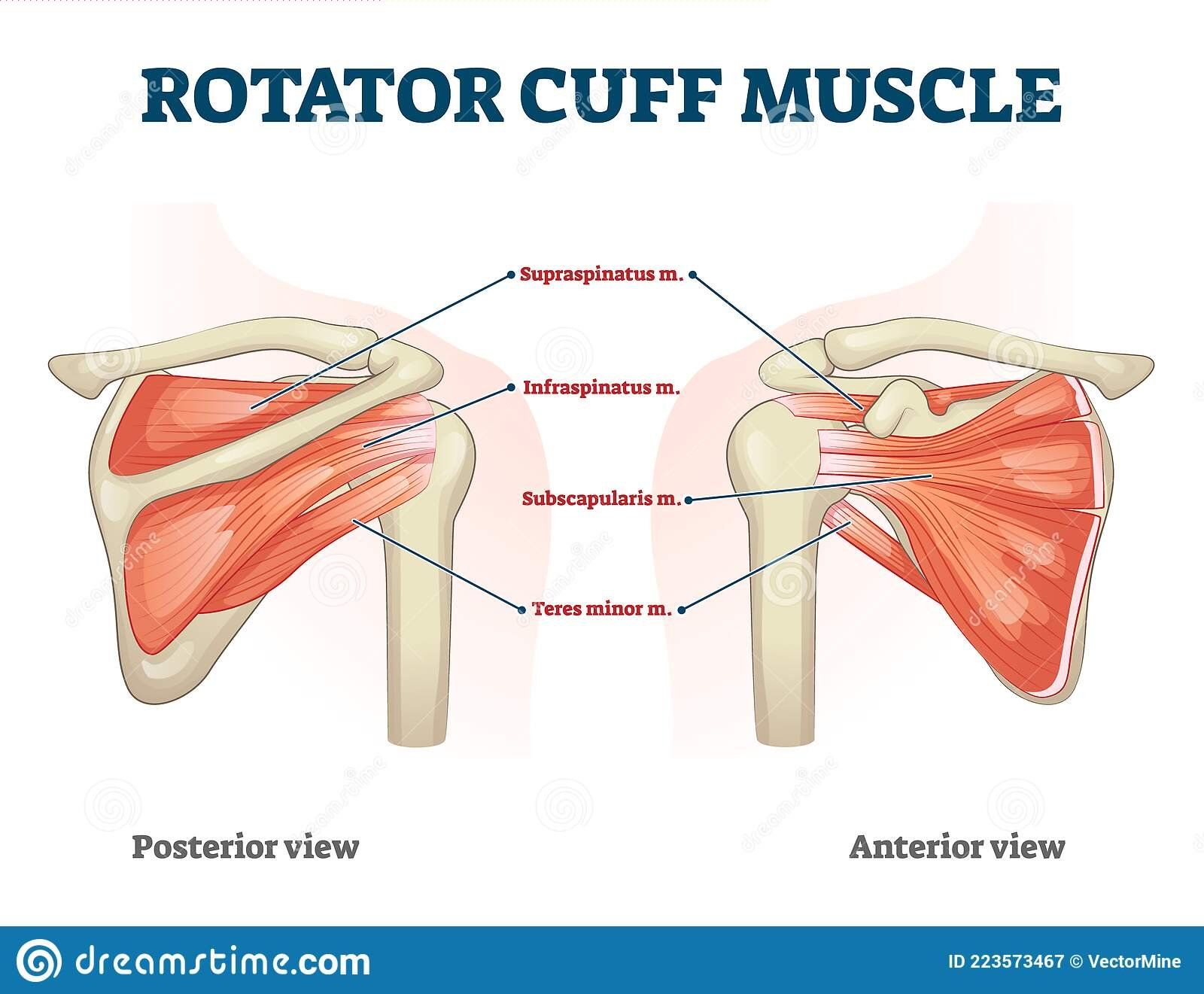
Recovery: Recovery time for a rotator cuff injury depends on the severity of the injury and the chosen treatment approach. With conservative treatment, most athletes can expect to return to their sport within several weeks to months, depending on their adherence to the rehabilitation program and the resolution of symptoms. Recovery from rotator cuff surgery can take several months, with a gradual return to throwing.
Ulnar Collateral Ligament (UCL) Injuries
Ulnar collateral ligament (UCL) injuries are prevalent among baseball players, particularly pitchers, due to the high stress placed on the medial (inner) aspect of the elbow during the throwing motion. The repetitive force and torque generated during throwing can lead to UCL injuries, ranging from mild inflammation to complete ligament tears.
Symptoms: UCL injuries may cause pain on the inner side of the elbow, swelling, and a sense of instability in the joint. A severe UCL injury can lead to a decreased ability to throw with the same velocity or accuracy, and in some cases, a "pop" or "snap" sensation might be felt during the injury.
Recovery: Recovery from UCL injuries depends on the severity of the injury and the chosen treatment approach. Non-surgical treatment may require several weeks to months of rest and rehabilitation, while recovery from Tommy John surgery typically takes 12-18 months before returning to competitive play.
Medial Epicondylitis (Golfer's Elbow)
Medial epicondylitis, or golfer's elbow, is an overuse injury resulting from the inflammation of the tendons that attach to the medial epicondyle of the elbow. This condition is often seen in baseball players, particularly pitchers and batters, due to the repetitive throwing and gripping motions involved in the sport.
Symptoms: Medial epicondylitis is characterized by pain and tenderness on the inner side of the elbow, which may worsen during throwing or gripping activities. In some cases, the pain may radiate down the forearm, and weakness in the hand and wrist may also be present.
Recovery: Recovery time for medial epicondylitis varies depending on the severity of the injury and the chosen treatment approach. With conservative treatment, most athletes can expect to return to their sport within several weeks to months, depending on their adherence to the rehabilitation program and the resolution of symptoms.
Lateral Epicondylitis (Tennis Elbow)
Lateral epicondylitis, also known as tennis elbow, is an overuse injury affecting the tendons that attach to the lateral epicondyle of the elbow. This condition is common among baseball players who frequently perform powerful wrist and forearm motions, such as batters and catchers.
Symptoms: Lateral epicondylitis is characterized by pain and tenderness on the outer side of the elbow, which may worsen during gripping or wrist extension activities. In some cases, the pain may radiate down the forearm, and weakness in the hand and wrist may be present.

Recovery: Recovery time for lateral epicondylitis varies depending on the severity of the injury and the chosen treatment approach. With conservative treatment, most athletes can expect to return to their sport within several weeks to months, depending on their adherence to the rehabilitation program and the resolution of symptoms.
Hamstring Strains
The hamstrings are a group of three muscles located at the back of the thigh, responsible for bending the knee and extending the hip. Baseball players can suffer hamstring strains due to the sudden acceleration and deceleration involved in running, base stealing, or making sudden stops.
Symptoms: Hamstring strains can vary in severity, from mild discomfort to severe pain and loss of function. Symptoms may include pain and tenderness at the back of the thigh, swelling, bruising, and difficulty bearing weight on the affected leg. In severe cases, a "pop" or "snap" sensation might be felt during the injury.
Recovery: Recovery time for a hamstring strain depends on the severity of the injury and the chosen treatment approach. With conservative treatment, most athletes can expect to return to their sport within a few weeks. Recovery from hamstring surgery from an avulsion fracture may take several months, with a gradual return to running and sports-specific activities.
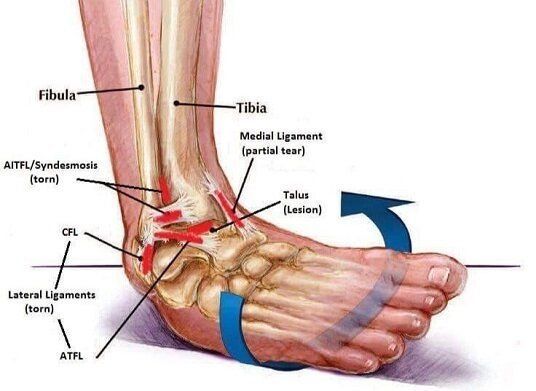
Ankle Sprains
Ankle sprains are common in baseball players due to the quick changes in direction and the uneven surfaces on the field. An ankle sprain occurs when the ligaments supporting the ankle joint are stretched or torn, resulting in pain, swelling, and difficulty bearing weight on the affected ankle.
Symptoms: Ankle sprains can vary in severity from mild to severe, depending on the extent of the ligament damage. Symptoms may include pain, swelling, and bruising around the ankle, as well as difficulty walking or bearing weight on the injured ankle. In more severe cases, the ankle may feel unstable or "loose.”
Rehabilitation and Prevention Strategies for Baseball Players
A comprehensive rehabilitation program for baseball players should address the specific needs of the athlete as an individual, their injury and what qualities they need to enhance to perform at their sport. This may include a combination of strength training, flexibility exercises, sport-specific drills, and a progressive return to play. It is essential to work closely with a sports physical therapist to ensure the rehabilitation program is tailored to the individual's needs and goals.
Warm-Up and Stretching
Incorporating a proper warm-up and stretching routine before practices and games can significantly reduce the risk of injuries in baseball players. Dynamic stretches and movements that mimic the sport's demands can help prepare the body for the stresses placed on it during play. These progressions may include personal corrective exercises, running drills (Mach Drills) and progressively increasing intensity of throwing and swinging.
Proper Throwing Techniques
Mastering proper throwing techniques can help minimize the risk of pain and injury. Working with a coach or sports professional to assess and correct any flaws in throwing mechanics can go a long way in preventing injuries associated with poor form. If you’re looking for coaching in the CT, we recommend choosing Swanson Baseball.
Strength and Conditioning
Developing a well-rounded strength and conditioning program can help baseball players build the necessary muscle balance, endurance, and power to perform at their best while reducing injury risk. It is essential to focus on exercises that target the muscles involved in throwing, hitting, and fielding, as well as core stability and lower body strength. If you’re looking for professional strength coaches who primarily works with baseball, we consider checking out LIFT Performance and Bold/T Performance.
Rest and Recovery
Adequate rest and recovery are crucial for preventing overuse injuries in baseball. This includes taking regular breaks during practices, allowing time for muscles to recover after intense workouts, and scheduling rest days to give the body time to repair and rebuild. Being honest with your body and with your coaching staff may be the difference between missing 1 game instead of the remainder of your season.

When to Seek Professional Help
While minor injuries can often be managed with rest, ice, compression, and elevation (RICE), it's essential to know when to seek professional help to ensure proper diagnosis, treatment, and recovery. Here are some signs that indicate it's time to consult a healthcare professional, such as a sports medicine physician, orthopedic specialist, or physical therapist:
- Persistent pain: If pain from an injury does not improve after several days of rest and self-care, or if it progressively worsens, it's a sign that you should seek professional help to determine the underlying cause and receive appropriate treatment.
- Recurring injuries: If you're experiencing frequent or recurring injuries, even if they seem minor, it's essential to seek professional help. Recurring injuries may indicate an underlying issue with your training, technique, or biomechanics, and a healthcare professional can help identify and address these issues to prevent future injuries.
- Swelling and inflammation: Moderate to severe swelling that does not improve after a few days or worsens may indicate a more serious injury, such as a fracture, dislocation, or ligament damage. In such cases, it's crucial to consult a healthcare professional for evaluation and treatment.
- Loss of function: If you are unable to move or bear weight on the affected joint or limb, or if you experience a significant loss of strength or range of motion, it's essential to seek professional help. These symptoms may indicate a more severe injury that requires medical intervention.
- Instability or deformity: If the injured area appears deformed, misaligned, or feels unstable, it's crucial to consult a healthcare professional immediately. These signs may indicate a fracture, dislocation, or severe ligament injury that requires urgent attention.
In summary, it's essential to listen to your body and recognize when your injury may require more than just self-care. Seeking professional help when necessary can not only ensure proper diagnosis and treatment but also help prevent complications and chronic issues that may impact your long-term athletic performance and overall health. Always err on the side of caution and consult a healthcare professional if you have concerns about your injury or recovery process.
Wrap Up
In conclusion, baseball players face various injuries due to the repetitive and high-impact nature of the sport. However, with proper prevention strategies, sports physical therapy, and rehabilitation, athletes can minimize their risk and recover more effectively from injuries. By focusing on warm-ups, proper techniques, strength and conditioning, and adequate rest, baseball players can enjoy a healthy and successful career on the field.
Frequently Asked Questions
1. What are the most common baseball injuries?
Some common baseball injuries include shoulder pain, pain with throwing, rotator cuff tears, tendinitis, and muscle strains.
2. How can I prevent baseball injuries?
Preventing baseball injuries involves incorporating proper warm-up and stretching routines, mastering throwing techniques, participating in strength and conditioning programs, and ensuring adequate rest and recovery.
3. When should I seek professional help for a baseball injury?
Seek professional help if you experience persistent pain, loss of range of motion, or a decrease in performance. A sports physical therapist or sports medicine physician can help diagnose and treat the underlying issue.
4. What does a sports physical therapy program for baseball players involve?
A sports physical therapy program for baseball players typically includes manual therapy, exercise therapy, throwing progressions, and a tailored rehabilitation plan focusing on the athlete's specific needs and goals.
5. How long does it take to recover from a baseball injury?
Recovery time for a baseball injury can vary depending on the severity of the injury, the individual's overall health, and the effectiveness of the rehabilitation program. It is essential to work closely with a sports physical therapist to ensure a safe and efficient return to play.










